Ocular surface squamous neoplasia encompasses
a broad spectrum of neoplastic abnormalities which include squamous dysplasia,
squamous cell carcinoma in situ, and invasive squamous cell carcinoma. Squamous cell carcinoma of the conjunctiva includes
neoplastic abnormalities that may cause severe morbidity to the patients. It is the third most common conjunctival
malignancy worldwide and is commonest in dark-skinned, Caucasians and in
tropics1. Its incidence is 37.3 per million
eyes with ocular tumors2. Thorough clinical assessment and early
diagnosis is the key for preventing the visual loss and morbidity in patients. Persons
in the older age group, those who have UV-light exposure and are smokers have
increased risk of developing ocular surface squamous neoplasia. Recurrence rate after surgical excision
within 2 years is 15-52% and associated with tissue disruption enhancing the
ability of tumor cells to enter in the eye. Previously,
mitomycin-C and 5-fluorouracil have been used with very good results but the
complications associated with these drugs have alarmed the physicians5.
The complications include uveitis, epithelial erosions, ulceration, and
glaucoma. Recent advances suggest use of Interferon-2bfor treating
these neoplasms6,7,8.Interferons
are glycoproteins that bind to cell receptors, and trigger effect or proteins
that inhibit viruses, activate immunocompetent cells and regulate oncogenes.
Interferon α-2b is a
recombinant form that has been used for hepatitis B/C, malignant melanoma,
follicular lymphoma, condylomaaccuminatum, Kaposi’s sacrcoma, multiple myeloma,
and hairy cell leukemia. The standard dose of topical interferon α-2B is 1M IU/ml. Median age for the complete
tumor resolution was three months. Few adverse effects of interferon α-2b are reported as photophobia, follicular
conjunctivitis, conjunctival hyperemia with foreign body sensation and pyogenic
granuloma. However, still it is better tolerated than the other forms of
topical therapies.
Rationale of the study was to analyze non-surgical
treatment of OSSN. Topical interferon alpha-2b therapy can be used to treat
OSSN (Immuno-therapy) as well as to reduce the size of OSSN (Immuno-reduction)
prior to excision. It may avoid the morbidity of excision that includes loss of
limbal stem cells or scarring of ocular surface. The
purpose of the study was to find the efficacy and
safety of topical and intra-lesional Interferon (IFN) α-2b for Ocular Surface Squamous Neoplasia (OSSN) in Pakistani population.
MATERIAL
& METHODS
This was a Quasi experimental study, which was conducted in Mayo hospital/KEMU Lahore,
Armed Forces Institute of Ophthalmology, Rawalpindi and Lahore General
Hospital, Pakistan from October 2010 to August 2016. Total Sample size of 90
patients was estimated by using 95% confidence level, 10% absolute precision
with expected percentage of Ocular surface squamous neoplasia as 91.6%.
n = (Z1-α/2)2
X P X q / d2
Z1-α2
= Confidence level 95% = 1.96
P = Prevalance
91.6%
q = 1-P
d = Absolute
precision 10%
Non-probability purposive sampling was done. The patients
with suspected conjunctival growths underwent incisional or excisional Biopsy
+/- cryotherapy. After histological confirmation of Ocular Surface Squamous
Neoplasia (OSSN) the case was included in the study. Patients with all other
forms of growths and patients with previous history of OSSN were excluded from
the study. All the pre- and post-operative data was recorded on a Proforma.
Intra-lesional/peri-lesional IFN α-2b was
injected weekly with a dose of 3 million IU along with interferon α-2btopical drops qid (1 MIU) until the resolution of
tumor. The drug was aspirated using a sterile syringe and transferred into an
emptied bottle of the artificial tears. The bottle was kept refrigerated until
used.
Only
those cases that completed at least 3 months follow-up after the resolution or
recurrence of lesion were included. Descriptive statistical results like
frequency and percentage was calculated by using SPSS Version 21.
RESULTS
Ninety-one eyes of 88 patients were included in study.
Out of these, 29 were females and 59 were males. The age of the patients was52-76
years (Mean 64 years). Eighty eyes tolerated and responded well to the
treatment and got cured. There was recurrence in 08 eyes (9.2%), all of which
had advanced squamous cell neoplasia. Three patients were lost to follow up.
Mean resolution time of tumor was 3 months and mean follow up time was 12
months with range of 3 months to 5 years.
The resolution time is shown in Fig-1.
The side
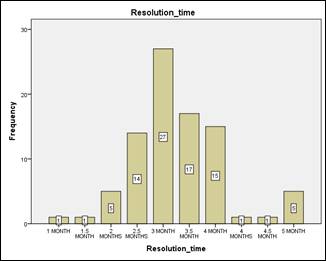
Fig. 1: Resolution Rate.
effects
recorded in our study were filamentary keratitis (1 patient), conjunctivitis (2
cases)and pyogenic granuloma (2 cases). Most of these resolved with lubricants.
However, the pyogenic granulomas needed excision under local anesthesia.
DISCUSSION
Ocular surface squamous neoplasia is the most common
malignancy in elderly patients, resulting in severe ocular damage and visual
impairment. We note that mean age of our study population was a bit younger
than those of Caucasian population.
Any lesion that is epithelial in origin mostly grows at the
limbus, because normal epithelial cellular activity is maximum at limbus9due
to the presence of Limbal Stem Cells.
The squamous cell carcinoma incidence varies
from 0.02 to 3.5 per 100,00010. In Conjunctival intra-epithelial
neoplasia (CIN/Bowen’s disease), basement membrane is not breached and lesion
is involving epithelial membrane only. If the tumor cells invade the basement
membrane and involve the sub-epithelial tissues, it is called Squamous cell
neoplasia.
Histological spectrum of squamous cell
carcinoma includes; micro-invasive, invasive, poorly differentiated and spindle
cell. Conjunctival and corneal surface can be involved with tumor, showing
dysplastic changes in epithelium from mild to moderate grade, and also of
infiltrative variety.
Previously, tumor was treated with excision leaving 2-3
mm tumor free margins, and cryotherapy was applied for the prevention of
recurrence11.Still, patients showed recurrence rate of6–30% with negative margins and up to 55% with
positive margins12. A study from Victoria (Australia)
reported death of 8% cases due to metastasis, despite orbital exenteration for
invasive OSSN13. In 18 patients reported from Pakistan, 42% needed
exenteration even after aggressive treatment of this tumor14. Therapy with antimetabolite agents like Mitomycin
C, 5-Fluorouracilhas been effective in treating the
small lesion and can be given as adjunctive therapy
following excision5 but have higher rate of recurrence.
On the other hand, recurrence rates after topical or injected interferon alpha-2b are
between 1% and 28%15,16 with follow-ups ranging from 2 to 28 months,
which is much lower. Our study also showed a similar recurrence rate (8.7%). Interferon α-2B has proven beneficial in small sized
localized lesions, large diffuse lesions and partially excised ocular surface
neoplasia, as well as in recurrent disease (Immunotherapy)15.
Analysis of 36 studies were published by Siedlecki
et al16and they concluded that excision of OSSN with positive
margins followed by topical Interferonα-2B is
the best strategy to reduce recurrence or persistent disease. In diseases that include extensive
involvement of ocular tissues, interferon asα-2b
can be used to reduce the size of the tumor (Immuno-reduction) so that after
excision there is less bare surface and lesser complications17.
Mitomycin-C, can result in corneal epitheliopathy,
corneal ulceration, dry-eye, uveitis and glaucoma. It has to be used as a tedious “on and off”
regimen, to prevent the complications associated with its continuous use12,17.
With the use of topical Interferon α-2b we came across very few side effects as compared to other
agents18. The side
effects we came across in our study were filamentary keratitis, conjunctivitis
and pyogenic granuloma formation, which were managed effectively. Most of the
time these resolved with lubricants, though pyogenic granuloma needed excision.
The major benefit of Interferon topical therapy is, that it obviates the need
of wide surgical excision. A study19 comparing the quality of life
in excision versus Interferonα-2bresulted
in similar outcomes.
This
topical medication is not available commercially in Pakistan hence, the drops
had to be dispensed in a sterile eye drops bottle. Patients should be counseled
about refrigeration and compliance of the therapy. The limitation in our study was a smaller population.
CONCLUSION
Intra-lesional
and perilesional Interferon α-2b
along with topical drops is a better option for the treatment of ocular surface
squamous neoplasia (OSSN) in our population. Future studies are needed to
determine the long-term effects.
ACKNOWLEDGEMENT
We
want to acknowledge Hafiza Ummara Rasheed COAVS Lahore for assistance in
statistical analysis.
REFERENCE
1.
Kaines A, Davis G, Selva D, Leibovitch I, Dodd T,
Malhotra R. Conjunctival
squamous cell carcinoma with perineural invasion resulting in death. Ophthalmic
Surg Lasers Imaging, 2005; 36 (3): 249-51.
2.
Basti S&Macsai MS. Ocular Surface Squamous Neoplasia: A Review. Cornea.
2003; 22 (7): 687-704.
3.
Ng J, Coroneo MT, Wakefield D, Di Girolamo N.Ultraviolet radiation and the role of matrix
metalloproteinases in the pathogenesis of ocular surface squamous neoplasia. Invest
Ophthalmol Vis Sci. 2008 Dec; 49 (12): 5295-306.
4.
Sen S, Sharma A, Panda A. Immuno-histochemical localization of human papilloma
virus in conjunctival neoplasias: a retrospective study. Indian J Ophthalmol.
2007; 55 (5): 361–3.
5.
C Chen, D Louis, T Dodd, J Muecke. Mitomycin C as an adjunct in the treatment of localised
ocular surface squamous neoplasia.Br J Ophthalmol. 2004; 88 (1): 17–18.
6.
Di Pascuale, Mario A, Espana, Edgar M, Tseng, Scheffer C.A Case of Conjunctiva-Cornea Intraepithelial Neoplasia
Successfully Treated with Topical Mitomycin C and Interferon Alfa-2b in Cycles;
Cornea. 2004: 23 (1): 89-92.
7.
Karp CL, Galor A, Chhabra S, Barnes SD, Alfonso EC. Subconjunctival/perilesional recombinant interferon α-2b for ocular surface squamous neoplasia: a 10-year
review. Ophthalmology, 2010; 117 (12): 2241-6.
8.
Kobayashi A, Yoshita T, Uchiyama K,Shirao Y, Kitagawa K,
Fujisawa A, Tseng SC. Successful
management of conjunctival intraepithelial neoplasia by interferon alpha-2b. JPN
J Ophthalmol. 2002; 46 (2): 215–7.
9.
Lee GA, Hirst LW. Ocular surface squamous neoplasia. Surv Ophthalmol.
1995; 39 (6): 429-450.
10. Yang
J, Foster CS.
Squamous cell carcinoma of the conjunctiva. Int Ophthalmol Clin. 1997; 37 (4): 73-84.
11. Fraunfelder
FT, Wingfield D. Management of
intraepithelial conjunctival tumors and squamous cell carcinomas. Am J
Ophthalmol. 1983; 95 (3): 359-63.
12. Daniell
M, Maini R, Tole D. Use of
mitomycin C in the treatment of corneal conjunctival intraepithelial neoplasia.
Clin Experiment Ophthalmol. 2002; 30 (2): 94-8.
13. McKelvie PA, Daniell M, McNab A,
Loughnan M, Santamaria JD. Squamous cell carcinoma of the
conjunctiva: a series of 26 cases. Br
J Ophthalmol. 2002; 86 (2): 168–173.
14. Siddiqui
ZK, Mahmood K, Lateef Q, Haider WA. Management of ocular surface squamous cell carcinoma at
Lahore General Hospital, Pakistan. Pak PG Med Jr. 2009; 20 (1): 30-31.
15. Boehm
MD, Huang AJ. Treatment of
recurrent corneal and conjunctival intraepithelial neoplasia with topical
interferon alfa-2b. Ophthalmology, 2004; 111 (9): 1755-61.
16.
Siedlecki AN, Tapp S, Tosteson AN, Larson RJ, Karp
CL, Lietman T, Zegan ME. Surgery versus interferon Alpha-2b treatment
strategies for ocular surface squamous neoplasia: a literature-based decision
analysis. Cornea, 2016; 35 (5):
613-618.
17. Kim HJ, Shields CL, Shah SU, Kaliki S, Lally SE. Giant ocular surface squamous neoplasia managed
with interferon alpha-2b as immunotherapy or immunoreduction. Ophthalmology,
2012; 119 (5): 938–44.
18. Galor A, Karp CL, Chhabra S, Barnes S, Alfonso EC. Topical interferon alpha 2b eye-drops for treatment
of ocular surface squamous neoplasia: A dose comparison study. Br J Ophthalmol.
2010; 94 (5): 551–4.
19.
Mercado CL, Pole
C, Wong J, Batlle JF, Roque F, Shaikh N, et
al. Surgical versus medical
treatment for ocular surface squamous neoplasia: A quality of life comparison. The ocular Surface, 2019; 17 (1):
60-63.
20.
McClellan AJ, McClellan AL, Pezon
CF, Karp CL, Feuer W, Galor A. The epidemiology of ocular surface
squamous neoplasia in a Veterans Affairs population. Cornea, 2013; 32 (10): 1354.